When it comes to fighting infections, Ofloxacin and Ornidazole are often the go-to antibiotics. These medications can work independently or as a powerful duo to tackle various bacterial and parasitic infections. And guess what? There’s even a combo pill to make life a little easier if both are prescribed. But, not everyone can take them—especially if you’re allergic to quinolone antibiotics. Let’s dive into how these meds work, when they’re used, and what you should know about potential side effects.
Breaking It Down: Ofloxacin and Ornidazole
What’s the deal with Ofloxacin?
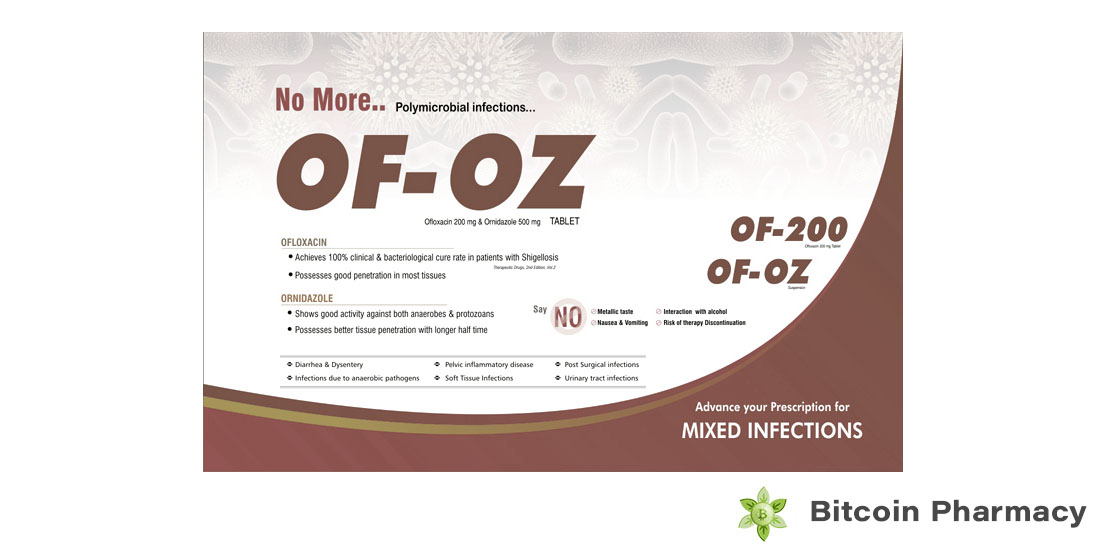
Ofloxacin is like the Swiss Army knife of antibiotics—it handles a bit of everything. It’s a fluoroquinolone antibiotic used for infections like UTIs, kidney and lung issues, and even sexually transmitted diseases like chlamydia and gonorrhea. Need something for eye or ear infections? Ofloxacin’s got your back. It’s also been used “off-label” for conditions like tuberculosis and corneal inflammation.
What about Ornidazole?
This one’s the expert in anaerobic and parasitic infections (think bacteria that don’t need oxygen). It’s perfect for handling intestinal infections, bacterial vaginosis, or even amoebic dysentery. Ornidazole can also be a preventative superstar, stopping infections before they even start—especially post-surgery.
When Two Become One: The Combination Therapy
Why combine them?
Together, Ofloxacin and Ornidazole pack a punch. They’re often prescribed for digestive tract infections causing abdominal pain or diarrhea. Got a stubborn UTI? This duo can help. From respiratory infections like pneumonia to certain STDs, this combination simplifies treatment—fewer pills, faster results, and less risk of resistance.
Even leprosy, a tough bacterial infection, benefits from this tag team. Doctors may use this pair along with other meds to shorten treatment time and reduce the spread of the disease. It’s all about efficiency!
Dosage: How Much Is Too Much?
For adults, the standard dose is one tablet (200mg Ofloxacin + 500mg Ornidazole) twice daily for 5–10 days. Kids under eight? They usually get a liquid suspension with the dosage depending on their weight. Either way, your doctor will tailor the treatment just for you.
Heads Up: Precautions You Should Know
Pregnant or breastfeeding?
These meds fall under category C, meaning there’s a “maybe” factor regarding safety. Make sure to consult your doctor if you’re expecting or nursing.
For kids:
Smallest dose, shortest time—that’s the rule for children.
The Not-So-Fun Part: Side Effects
Like most meds, these antibiotics come with a list of possible side effects. While common issues like nausea, headaches, and dizziness might be manageable, some side effects could raise red flags. Think severe allergic reactions, abnormal heart rhythms, or tendon ruptures. Pairing these drugs with corticosteroids? That might amplify risks. Always talk to your doctor if anything feels off.
At the end of the day, Ofloxacin and Ornidazole are powerful tools for fighting infections. But like any tool, they need to be used carefully and wisely. Always follow your doctor’s advice, and don’t hesitate to ask questions. After all, it’s your health!